Although Abdi Ali* was released from prison in June this year, he remains a prisoner of the disease he contracted there.
He served one year for assault and contracted tuberculosis (TB) in the prison’s overcrowded cells.
His lungs are scarred and he developed resistance to the common antibiotics used to treat TB.
He is lucky to be alive because many prisoners with TB die before they taste freedom.
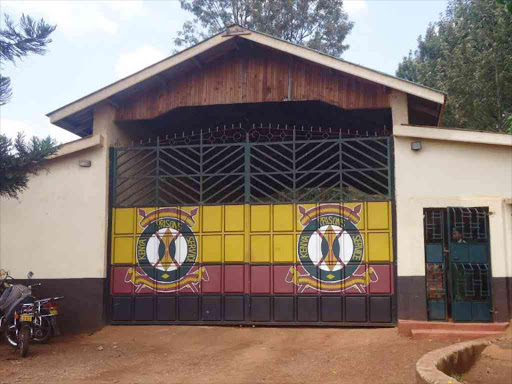
In June last year, a team of investigators visited Shimo La Tewa prison, where Ali (real name changed to protect identity) was incarcerated, to determine the number of inmates infected with TB and HIV.
The researchers tested all adult inmates presenting with signs and symptoms suggestive of TB for the disease.
The overall prevalence of TB among inmates with presumptive pulmonary TB was 10.2 per cent. All of the TB patients were HIV positive.
Their findings, published last month, underscore a grim reality: TB prevalence in prisons is more than 10 times higher than in the general population.
“Inmates with TB can serve as hotspots for TB transmission within prison walls and outside communities after their release, highlighting the public health importance of interventions targeting this key population in national and global efforts to eradicate TB,” the researchers said.
They published their findings last month in the Tropical Medicine and Health journal in a paper titled ‘Prevalence and associated factors of TB and HIV coinfections among adult inmates with presumptive pulmonary TB in a Kenyan prison’.
The link between TB and HIV is particularly concerning, as the coinfection accelerates the decline of the immune system, leading to higher mortality rates if left untreated.
“The high TB burden in prisons is attributable to low health services priorities by public health policymakers, infrastructural designs that favour overcrowding with no sufficient ventilation, and prisoners’ vulnerability due to malnutrition, HIV infection, smoking and alcohol use disorders,” the researchers said.
The authors said prisoners who are underweight or have a history of smoking or illegal drug use were at significantly higher risk of developing TB and HIV coinfections.
Specifically, prisoners with a history of illegal drug use were found to be five times more likely to harbour TB and HIV coinfections compared to those without such a history.
Smoking also emerged as a critical factor, with inmates who smoked, being three times more likely to have a TB and HIV coinfection.
Education emerged as a protective factor against TB and HIV coinfections. The study revealed that prisoners with primary or secondary education were 83-85 per cent less likely to develop these infections compared to those without formal education.
“The authorities should take measures to protect HIV-positive prisoners from TB, focusing on education, nutrition, smoking, and illegal drug use. Multicentric studies with large sample sizes are needed to substantiate the findings further,” the authors said.
Despite being a single-centre study with a small sample size (157 adults), which may limit the generalisation of the findings in similar settings, the research offers insight into the significant burden of TB and HIV coinfections in Kenya prisons.
Prisons rarely factored in national disease surveillance and data to inform TB control interventions in correctional facilities is limited.
The authors are from Moi Referral Hospital in Voi and Kenyatta University.
They said their findings point to an urgent need for systematic and continuous surveillance of TB and HIV in prisons, especially in resource-constrained settings like Kenya, where prisons are often excluded from national health statistics.
The researchers called for immediate action to protect HIV-positive prisoners from TB by focusing on improving education, nutrition and addressing issues related to smoking and illegal drug use.